Innhold
- McKenzie-metoden
- Nedre ryggplager (LBP)
- Undersøkelse McKenzie
- Klassifisering McKenzie
- Behandling McKenzie
- Forskning om McKenzie
- Referanser
Introduksjon
McKenzie-metoden eller Mekanisk Diagnostikk og Terapi (MDT) er en internasjonal annerkjent metode for diagnostikk og behandling rettet mot ryggrad og ekstremitetssmerter. Metoden ble utviklet av fysioterapeut Robin McKenzie i 1956 av en tilfeldig pasientkasuistikk som dannet grunnlag for utvikling av teorier og klinisk praksis av protokoller for behandling av mekanisk induserte smerter i ryggraden. I et intervju om hvordan den konseptualiseringen fant sted, forteller McKenzie følgende:
“My first experience with what I have chosen to call the ‘Centralisation Phenomenon’ occurred in 1956. A patient, ‘Mr Smith’, who had pain to the right of the low back, extending into the buttock and thigh to the knee, had undergone treatment for three weeks without improvement. He could bend forwards, but could not bend backwards. I told him to undress and lie face down on the treatment table, the end of which had been raised for a previous patient. Without adjusting the table, and unnoticed by any of the clinical staff, he lay face down with his back overstretched for some five minutes. After some time, when I entered the room I was aghast to find him lying in what at that time was considered to be a most damaging position. On enquiring as to his welfare, I was astounded to hear him say that this was the best he had been in three weeks. All pain had disappeared from his leg. Furthermore, the pain in the back had moved from the right side to the centre. In addition, his restricted range of extension had markedly improved. After standing upright, the patient remained improved with no recurrence of leg pain. The position was adopted again the following day and resulted in complete resolution of central low back pain. The movement of pain from the leg or buttocks to the middle of the back is now known as the centralisation phenomenon.”
MDT brukes i dag av flere profesjoner (se lengre ned praksisforskjellen), men i bunn og grunn brukes det av MDT-praktikere til å evaluere, diagnostisere og behandle problematikk i og rundt om ryggraden, ledd og muskler. Hjertebarnet til McKenzie ligger i mobiliseringsøvelser og filosofien bak MDT ligger i «aktiv pasientinvolvering og skolering». Hovedelementet i MDT er førstegangsevalueringen som ligger til grunnn for en behandlingsplan. MR anvendes anvendes som regel ikke. McKenzie-metoden er relativt utbredt på verdens basis og det som kjennetegner metoden for majoriteten som er fortrolig med MDT eller anvender det i deres kliniske praksis, er at det er et sett med øvelser for rygg- og/eller nakkesmerter som pasienten kan utføre på egenhånd som et ledd av et behandlingsforløp. Dette er delvis sant, men for en MDT-praktiker består McKenzie-metoden av flere ledd; 1) Undersøkelse, 2) Behandling og 3) Forebygging. Dette innebærer i utgangspunktet et lukket system bestående av de tre elementene for at McKenzie-metoden skal praktiseres i sin helhet. Likevel benyttes McKenzie-metoden av andre profesjoner innenfor muskel-skjellett rehabilitering, inkludert bl.a Manuelterapeuter og Spesialister i Klinisk Ortopedisk Fysioterapi (ad modum Cyriax), som benytter seg av deres eget diagnostisk system og verktøy, men kan anvende McKenzie-behandling i form av aktive mobiliseringsøvelser der pasienten blir invovelsert aktivt i behandlingen.
Mekaniske Nedre Ryggplager (LBP)
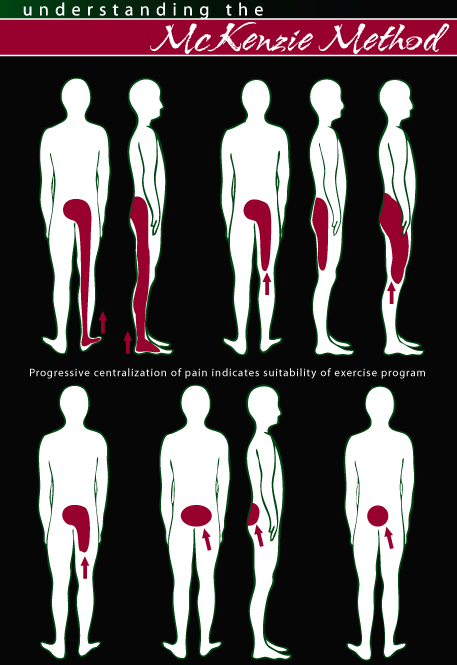
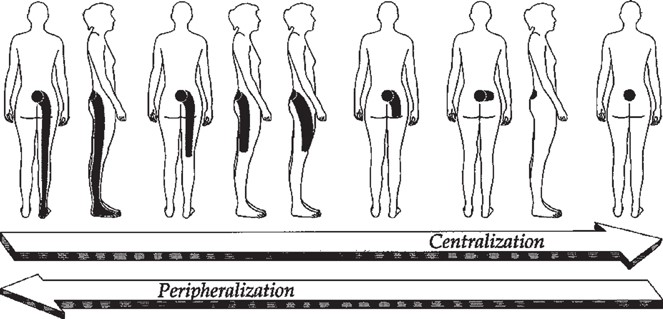
Det mest fundamentale av McKenzie tilnærmingen er behandling som eksponerer ryggraden for strekk og resulterer i smertelindring av smertereferansen ut i ekstremitetene (arm eller bein) og «sentralisering» av dem ved ryggraden. Tanken bak sentralisering av smertene er å forsøke å behandle årsaken enn bare symptomene. I følge McKenzie-metoden skal det være rom for egen tilheling uten hjelp av passive modaliteter som f.eks varme, kulde, medisinering eller nåler. I det lange løpet sikter metoden seg på å skolere nakke/rygg-pasienter til å behandle seg selv og til å håndere plagene ved å bruke øvelser og andre strategier. Målsetningen består av:
- Rask smertelindring
- Komme tilbake til daglige aktiviteter og gjennopprette funksjon
- Forebygge risiko for tilbakefall (posturale endringer elller aktiviteter)
Smerteforflyttingen bak «sentraliseringsprinsippet» til McKenzie vil ikke være tilfelle for alle pasienter eller tilstander. Derfor er behandling i form av ekstensjonsbehandling utelukkende rettet for pasienter der smertene sentraliseres. Dette er viktig å ta i betraktning da enkelte tilstander; sentral stenose lumbalt, facetleddsartritt, vil oppleve forverring av smertetilstanden ved eksponering for lignende behandling.
I følge McKenzie-metoden klassifiseres tilstandene basert på symptomene og responsen kartlagt under den initielle undersøkelsen. Basert på den klassifiseringen, instrueres pasienten i spesifikke øvelser som har til hensikt å sentralisere eller lindre smertene. Følgende tre mekaniske klassifiseringer betynnes av McKenzie-metoden for å gruppere ift behandling; Postural syndrom, Dysfunksjonell syndrom og Derangement syndrom. Alle tre er beskrevet nedenfor (se Klassifisering).
I videoen nedenfor beskrives metoden i sin aller første form direkte av Robin McKenzie, men gjennom årene har noe av innholdet og tilnærmingen endret seg.
Undersøkelse ad modum McKenzie
Riktig undersøkelse bygger grunnlag for valg av riktige mobiliseringsøvelser ad modum McKenzie. Uten riktig undersøkelse basert på mekanisk induserte smerter, finnes det ikke McKenzie øvelser, men bare øvelser der effektivitet kan være av utfordring å kartlegge. Når symptomene som initielt er kartlagt endres i en positiv retning ved at pasienten inntar forskjellige aktive stillinger, defineres dette i følge McKenzie som en «preferert bevegelsesretning» mtp behandling. Identifisering av nemlig preferanse av bevegelsesretning (directional preference of movement) gjennom biomekaniske prisipper kjennetegner McKenzie-metoden, også omtalt som Mekanisk Diagnostikk og Terapi (MDT).
Den prefererte bevegelsesretningen er også den retningen som resulterer i at smertene forflyttes seg sentralt (sentraliseringsprisippet beskrevet ovenfor), og smertereferanse ut i ekstremitetene avtar.
Røde Flag
Undersøkelse består av kartlegging av anamnetiske funn og skadehistorie, samt klinisk undersøkelse. Begge elementene ligger til grunn for å identifisere røde flag som kan være i og for seg kontraindikasjon for øvelsesbasert behandling. Disse innebærer spinalfraktur, spinalkreft, spinale infeksjoner og systemiske inflammatoriske tilstander. McKenzie-metoden innebærer en bevegelsesrettet undersøkelse der pasienten eksponeres for spesifikke bevegelser som har til hensikt å evaluere om smerter provoseres eller lindres (se preferert bevegelsesretning ovenfor), eksempelvis utførelse av enkel og repetitiv fleksjon eller eksensjon og kartlegging av forverring eller lindring av smerter;
- Smerter sentraliserer seg mer lokalt i ryggen og smertereferanse i ekstremitetene avtar eller forsvinner.
- Smerter oppleves mer perifert ut i ekstremitetene.
Lateral fleksjon ipsi- eller kontralateralt til smerteområde kan også bli undersøkt. Bevegelsene er viktig å bli utført til end-range (ytre stilling) der en ikke får hente ut mer utslag, samt i både liggende og stående stilling. Når retningspreferanse, mao bevegelser som resulterer i smertelindring, er identifisert, klassifiseres pasienten ift tilstand og respektive McKenzie øvelser tas i bruk. Undersøkelsesskjema for de nedenforlistet områdene finnes direkte på Mckenzie Institutt nettisiden og brukes etter McKenzie retningslinjer;
Klassifisering ad modum McKenzie
Systemet i Mekanisk Diagnostikk og Terapi har en tredelt klassifisering av makniske tilstander og sub-klassifisering innad de gruppene;
1) Postural syndrom; Omfatter ryggplager indusert av kontinuerlig belastning av bløtvev ved spesifikke kroppsholdninger. En lignende tilstand er i følge McKenzie et resultat av langvarig eksponering for spesifikke kroppsholdninger og posisjoner som kan affisere leddflater, muskler og seneaparatt. Smerter er reproduserbare og av lokal karakter når ytre stillinger opprettholdes over en tidsperiode. Repeterte bevegelser vil ikke endre symptobilde hos en pasient med postural syndrom og respons forventes til å være umiddelbar. Ved en lignende tilstand utføres det kroppsholdninger som er med på å reprodusere symptombildet pasienter har i utgangspunktet beskrevet, etterfulgt av kroppsholdninger som er med på å lindre symptomene. Dette benyttes for å illustrere hva som kan fremkalle plagene og dermed forklare at unngåelse av disse i første omgang kombinert med andre øvelser kan være et gunstig utgangspunkt.
2) Disfunksjonell syndrom: ryggplager med bevegelseshemming provosert av arrvev i forkortet tilstand; smerter oppstår når bløtvevet blir utsatt for belastning. Den disfunksjonelle klassifiseringen omfatter adaptive forkortninger, arrvev eller adheranser av bløtvev som ligger til grunn for smertene. Lignende kan være forbigående, tilbakevendende eller kronisk. Disse innebærer f.eks lignende tilstander indusert etter kirurgiske inngrep (se lumbal laminectemi, microdisectomi og epidural fibrosis). Kjennetegn for lignende er smerter ved ytre stillinger. Bevegelse vekk fra ytre stillinger lindrer smertene. I følge McKenzie vil behandling av lignende være tidskrevende da vevremodulering er tidskrevende. Samtale om smerteforklaring og pasientskolering er viktige, da det innebærer at vedkommende at prosessen rundt remodulering av vev kan være tidskrevende, samt at øvelser har til hensikt å forsøke å assistere behandling av adheranser rundt om og i bløtvevet.
3) Derangement syndrom: ryggplager indusert av bevegelse ved aktuell virkel/disk og forflytting av diskens innhold; smerter vil endre seg ved repetiviv bevegelse. Denne tilstanden er den vannligste i sin klinisk presens. Kjennetegn for denne tilstanden er smertereproduksjonen for enkelte bevegelsesmønstre og smertelindring under andre bevegelsesmønstre; når henholdsvis fleksjon eller ekstensjon blir brukt kartlegges det om symptomene følger sentraliseringsprisippet. Mao om smertene avtar i ekstremitetene og blir bare lokalt i ryggen, eller om smertene blir mer intense ut i ekstremitetene.
Behandling ad modum McKenzie
Behandling ad modum McKenzie har to aktive elementer som består av;
McKenzie-øvelser basert på symptombilde, undersøkelse og klassifisering. Målsetningen handler om å sentralisere smertene, der smertene forsvinner i første omgang fra ekstremitetene og er mer lokalisert lokalt i f.eks nedre rygg før de forsvinner helt.
Pasientskolering rundt smerter og symptombilde er essesielt. Det er viktig for pasienten å vite mer om tilstanden, hensikten med øvelsene og tiltak for forebygging av fremtidige evt tilbakefall. Pasinten ønskes å være en aktiv del av behandlingen.
McKenzie-øvelser, sentralisering og forventet resultater
Når klassifisering er kartlagt og preferert bevegelsesretning (se def. og beskrivelse av det lengre opp) er kjent, planlegges det øvelser som skal ramme behandlingen. Målet, som nevnt tidligere, er å sentralisere smertene med et overordnet mål om å behandle årsaken, istedenfor å behandle perifert; smertereferanse ut i ekstremiteter. Smertene forventes til å enten lindres eller fosvinne gjennom øvelser utført på daglig basis.
1) Ektensjon som preferert bevegelsesretning
Om strekk i f.eks ryggraden viser seg til å forandre symptombilde ved at smertene ut i underekstremiter forsvinner og smertene lokaliseres mer lokalt i nedre rygg, følgende McKenzie-øvelser er brukt i behandlingen;
- Behandling kan starte i liggende posisjon (dette er individuelt og avhenger av symptombilde kartlagt under undersøkelsen).
- For postural syndrom: Fokus på holdningskorrigerende tilstand gjeldende sittende og stående stilling er viktige. Øvelsene ligner de til disfunksjonell syndrom, men avhenger av symptombilde
- For disfunksjonell syndrom: Fokus på behandling er remodullering av bløtvev og omfatter øvelser i mageliggende, progresjon over til mageliggende med støtte på albuene og til slutt i mageliggende med støtte på armene med fult strekk i armene.
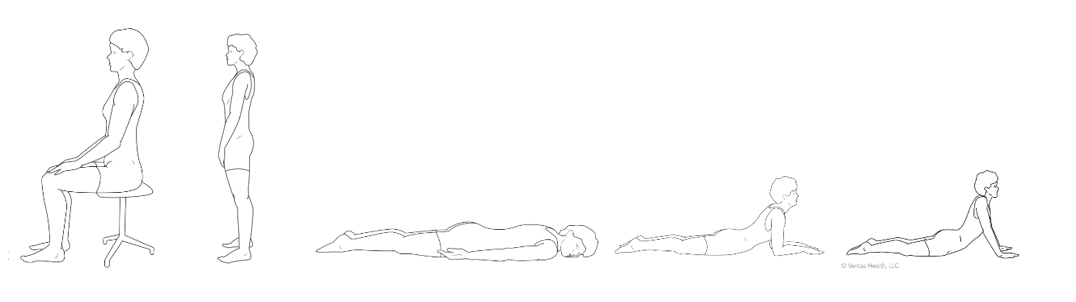
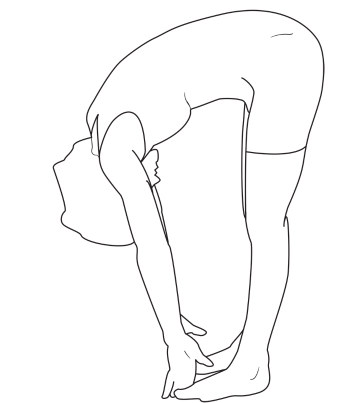
2) Fleksjon som preferert bevegelsesretning
Om strekk i f.eks ryggraden viser seg til å forandre symptombilde ved at smertene ut i underekstremiter forsvinner og smertene lokaliseres mer lokalt i nedre rygg, følgende McKenzie-øvelser er brukt i behandlingen;
- I liggende
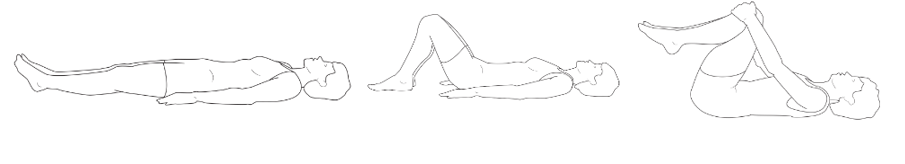
- I sittende

- I stående
Forskning om McKenzie-metoden
Forskningsliteratur revelant til McKenzie-metoden samlet og gruppert av Stephen May. Dette for å kunne få oversikt over literaturbelegg bak metoden. Samlet oversikt over artikler finnes også på McKenzie instituttet sin nettside. Artikler markert med * refererer til artikler med betydning for klinisk undersøkelse og behandling i følge Stephen May.
- Lumbar Spine - Systematic Reviews
- Lumbar Spine - Reviews
- Lumbar Spine - Trials using McKenzie or Flexion/Extention regimes
- Lumbar Spine - Surveys of McKenzie regimes & Use of McKenzie Method
- Lumbar Spine - Assessment procedures, Tests & Techniques
- Lumbar Spine - Anatomical Physiological & Pain Studies
- Lumbar Spine - Overviews
- Lumbar Spine - Discussion Articles
Belanger A Y, Depres M C, Goulet H, Trottier F; The McKenzie Approach: How Many Clinical Trials support Its Effectiveness? Proceedings of the World Confederation for Physical Therapy 11th International Congress, 28 July – 2nd August 1991, London, UK.
A review and analyses of the scientific literature that supports the effectiveness of the McKenzie approach. It concludes that despite worldwide popularity, scientific validation of the method is still not available.
Faas A, Exercises. Which ones are worth trying, for which patients, and when? Spine, 21, 24, 2874-2879, 1996
A review of eleven randomised exercise trials concerning exercise therapy. Two trials of McKenzie type exercises reported positive results but had low method scores.
Koes B W, Bouter L M, Beckerman H, van der Heijden G J M G, Knipschild P G: Physiotherapy exercises and back pain: a blinded review. BMJ 302;1572-1576, June 1991.
Koes concludes that the quality of research on the effect of exercises in the treatment of LBP is disappointingly low and, therefore, no conclusion can be drawn on whether exercise is better than other treatments or whether a specific type of exercise is more effective.
Reddeck T: The Efficacy of the McKenzie Regimen – A Meta-analysis of Clinical Trials. Proceedings of 10th Biennial Conference of the Manipulative Physiotherapists Association of Australia. Melbourne, Australia, 156-161, November, 1997.
Finds some support for the efficacy of McKenzie regimen, but the limited number of trials and their poor methodology make it impossible to draw firm conclusions.
Van Tulder Mw, Koes BW, Bouter LM: Conservative treatment of acute and chronic nonspecific low back pain. A systematic review of RCT of the most common interventions. Spine 22;2128-2156, 1997.
Probably the most thorough recent systematic review of a wide range of treatments. Amongst their findings – exercise therapy for acute back pain is ineffective; exercise therapy for chronic back pain is effective, but with no clear evidence in favour of any particular form of exercise.
Delaney PM, Fernandez CE:Toward an evidence-based model for chiropractic education and practice. J Manip & Physio Thera 22;114-118, 1999.
This commentary outlines the steps of evidence-based health care – formulating a question; searching the literature; critically appraising the literature; managing the patient accordingly; evaluating one’s own practice. As an example of critical appraisal they examine Donelson (1997) and conclude that the McKenzie protocol is a useful, highly sensitive, and moderately specific diagnostic tool for discogenic pain and annular incompetency.
DiMaggio A, Mooney V: Conservative care for low back pain; what works? Journ Musculoskel Med 4:9;27-34, 1987. A review of conservative therapy and an introduction to the McKenzie individualised prescription of exercises aimed at influencing the mechanical source of pain.
Fast A: Low Back Disorders: Conservative management. Arch Phys med Rehabil, Vol 69;880-891, 1988.
Following relevant anatomical considerations, the many causes of LBP are outlined. The McKenzie approach is included as one of the many conservative treatment measures.
Frost H, Moffett J K: Physiotherapy Management of Chronic Low Back Pain. Physiotheraphy 78:10;751-754, 1992.
A review of the psychological and physical benefits of an active, patient controlled treatment regime compared to passive modalities.
Huijbregts PA: Fact and fiction of Disc Reduction: A Literature Review. J Manual & Manip Therapy 6:137-143, 1998.
This review examines the effect of manipulation, traction, and McKenzie exercises on the position of herniated nuclear material in lumbar intervertebral discs. From the evidence reviewed the author concludes that there is no proof that rotatory manipulation is effective and may lead to further displacement; that traction may temporarily influence displacement; and that extension exercises may influence displacement in non-degenerated discs, but does not allow conclusions about the effect in degenerated or herniated discs.
McKenzie R A: REPEX in Acute and Subacute Low back Pain. In: Proceedings of Advances in Idiopathic Low Back Pain Symposium, Vienna, Austria, Nov 27-28, 1992. Ed Prof DDr E Ernst.
This article introduces the REPEX and includes a review of the use of end of range passive exercises and the literature pertaining to the method.
Mooney V: Herniated discs. In: Automated Percutaneous Lumbar Discectomy. Eds G Onik, C A Helms. San Fransisco: Radiology research and Education Foundation, 1988:53-70.
Mooney discusses herniated disc pathology and diagnosis, followed by conservative and surgical treatment options. The McKenzie method and studies that support it are included under conservative care.
Adams N.: Psychophysiological and Neurochemical Substrates of Chronic Low Back Pain and Modulation by treatment. Physiotherapy 79:2;86, 1993
Chronic low back pain patients had decreased pain scale readings, increased lumbar range of motion, reduced EMG activity, and elevated levels of substance P following a 6 week treatment programme of McKenzie extension procedures.
Alexander A H, Jones A M, Rosenbaum Jr D H: Nonoperative Management of Herniated Nucleus Pulposus: Patient Selection by the Extension Sign – Long-term Follow-up. Orthop Trans 15:3;674, 1991.
Long term follow-up revealed that a negative extension sign is a good predictor of a favourable response to non operative treatment in 91% of patients with herniated nucleus pulposus.
Buswell J: Low back pain: a comparison of two treatment programmes. NZ J of Physiotherapy 13-17 August, 1982.
Patients were treated by extension or flexion protocols, both produced significant improvements in patient outcomes, with no difference between the 2 groups.
Cherkin DC, Deyo RA, Battie MC, Street JH, Hunt M, Barlow W, A Comparison of Physical Therapy, Chiropractic Manipulation or an educational booklet for the treatment for low back pain. NEJM 339:.1021-1029, 1998.
McKenzie therapy and chiropractic manipulation are equally effective and both are slightly superior to the booklet in terms of patient satisfaction and short-term symptom reduction. The long-term outcome measures were the same in all 3 groups, including recurrences and care-seeking. The cost of the booklet group was considerably less than the 2 other groups.
Delitto A, Cibulka M T, Erhard R E, Bowling R W, Tenhula J A: Evidence for use of an extension-mobilization category in low back syndrome: a prescriptive validation pilot study. Physical Therapy 73:4;216, 1993.
Delitto suggests that treatment strategy based on signs and symptoms and response to movement may result in a more effective outcome compared with an unmatched non-specific treatment. Patients classified as extension-responders did better with an extension, than a flexion oriented programme.
Dettori JR, Bullock SH, Sutlive TG, Franklin RJ, Patience T: The Effects of Spinal Flexion and Extension Exercises and their Associated Postures in Patients with Acute Low Back Pain. Spine 20:21;2303-2312, 1995.
In the first week both exercise groups improved more than the control group. Subsequent to that there was no significant difference between the groups. Recovery of all groups was generally rapid, but recurrence was frequent.
* Donelson R, Murphy K, Silva G: Centralisation Phenomenon: Its usefulness in evaluating and treating referred pain. Spine 15:3, 211-213, 1990.
The centralisation phenomenon is found to be a reliable predictor of good or excellent treatment outcome. In 87 patients centralisation occurred in 87% – with centralisation occurring in 100% of 59 patients with excellent outcomes.
* Donelson R, Grant W, Kamps C, Medcalf R: Pain Response to Sagittal End-Range spinal Motion: A Prospective, Randomized Multicentered Trial. Spine 16:6S;S206-S212, 1991.
Donelson found that 47% of low back pain patients with or without referred pain displayed a directional preference to end range sagittal spinal movement – 40% preferred extension, 7% preferred flexion.
* Donelson R G; Grant W D et al: Low Back and Referred Pain Response to Mechanical Lumbar Movements in the Frontal Plane. Presented at International Society for the Study of the Lumbar Spine Meeting, Heidelberg, May 12-16, 1991.
Centralisation can be achieved with end range frontal plane spinal movements in a majority of patients who failed to centralise with sagittal plane movements.
Elnaggar I M, Nordin M, Sheikhzadeh A, Parnianpour M, Kahanovitz N: Effects of Spinal Flexion and Extension Exercises on Low-Back Pain and Spinal Mobility in Chronic Mechanical Low-Back Pain Patients. Spine 16:8;967-972, 1991.
Flexion and Extension exercises in a chronic low back pain population decreased pain levels and increased sagittal movement with no obvious preference to direction.
Erhard RE, Delitto A, Cibulka MT: Relative Effectiveness of an Extension Program and a Combined Program of Manipulation and Flexion and Extension Exercises in Patients with Acute Low Baxk Syndrome. Physical Therapy, 74:12;1093-1100, 1994.
Manipulation and general exercise group had greater improvements than pure extension group.
Faas A, Chavannes AW, van Ejik JTM, Gubbels JW: A Randomized, Placebo-Controlled Trial of Exercise Therapy in Patients with Acute Low Back Pain. Spine 18:11;1388-1395,1993.
No differences in outcomes were found between groups receiving flexion exercises and advice, placebo ultrasound, or usual GP care.
Fredrickson B E, Murphy K, Donelson R, Yuan H: McKenzie Treatment of Low back Pain: a correlation of Significant Factors in Determining Prognosis. Annual meeting of International Society for the Study of the Lumbar Spine, Dallas Texas, USA, 1986.
In a large patient population, categorisation and treatment according to the McKenzie system is found to have definite prognostic value.
Gilbert JR, Taylor DW, Hildebrand A, Evans C: Clinical Trial of Common Treatments for Low Back Pain in Family Practice. BMJ 291;791-794, 1985.
Bed rest, flexion exercise group with advice, and control group all had similar outcomes.
Gillan MG, Ross JC, McLean IP, Porter RW. The natural history of trunk list, its associated disability and the influence of McKenzie management. Euro Spine J 7.6.480-483, 1998.
Patients with a trunk list were randomised to McKenzie protocol or non-specific back care. At 90 days there was a significantly greater reduction of list in the McKenzie group, but no clinical difference. List and functional disability were poorly correlated.
* Kopp J R, Alexander A H, Turocy R H, Levrini M G, Litchman D M: The use of Lumbar Extension in the Evaluation and Treatment of Patients with Acute Herniated Nucleus Pulposus. A preliminary Report. Clinical Orthopaedics 202:211-218, January 1986.
The ability to achieve full passive extension correlated with good response to conservative treatment.
* Long A, The Centralisation Phenomenon. Its usefulness as a predictor of outcome in conservative treatment of chronic low back pain. Spine, 20, 23, 2513-2521, 1995.
A pilot study indicating that centralisation is useful as an outcome predictor in chronic patients. There was a superior outcome comparing centralisers to non-centralisers in an interdisciplinary work-hardening programme.
Malmivaara A, Hakkinen U, Aro T et al: The Treatment of Acute Low Back Pain – Bed Rest, Exercises, or Ordinary Activity? New England J Med. 332:6;351-355, 1995.
Ordinary activity group had significantly better outcomes than those prescribed bed rest, or extension and lateral bending exercises.
Nwuga G, Nwuga V: Relative therapeutic efficacy of the Williams and McKenzie protocols in back pain management. Physiotherapy Practice 1:99-105, 1985.
A treatment trial of McKenzie versus Williams protocol favours the McKenzie approach in patients with a diagnosis of disc prolapse.
Ponte D J, Jensen G J, Kent B E: A Preliminary Report on the use of the McKenzie protocol versus Williams Protocol in the treatment of Low Back Pain. Journ Orthop & Sports Phys Ther, Vol 6:2;130-139., 1984
In LBP patients, the McKenzie protocol was superior to the Williams protocol in decreasing pain and hastening the return of painfree range of motion.
Roberts A P: The conservative treatment of low back pain. (Thesis) Nottingham 1990.
At 7 weeks post onset of LBP, Roberts showed that the group receiving McKenzie treatment produced significant disability reduction compared with those treated with a NSAID (Ketoprofen).
Saal JA, Saal JS: Nonoperative treatment of herniated lumbar intervertebral disc with radiculopathy. Spine 14:4;431-437.
64 patients with herniated nucleus pulposus, including those with extrusions, were treated conservatively with a regime that included extension exercises, injections, lumbar stabilisation exercises, and a general exercise programme. The majority of patients had good or excellent outcomes, with failure to respond associated with stenosis.
* Snook SH, Webster BS, McGorry RW, Fogleman MT, McCann KB: The reduction of Chronic Nonspecific Low Back pain through the control of early Morning Lumbar Flexion. RCT. Spine 23:2601-2607, 1998.
Education in the control of early morning flexion produced significant reductions in pain intensity, days in pain, disability and medication use. High drop-out rates show the difficulty of getting people to make such behavioural changes.
* Spratt KF, Weinstein JN, Lehmann TR, Woody J, Sayre H: Efficacy of Flexion and Extension Treatments Incorporating Braces for Low-Back Pain Patients with Retrodisplacement, Spondylolisthesis, or Normal Sagittal Translation. Spine 18:13;1839-1849, 1993.
Improvement in the extension group was significantly greater, regardless of type of radiographic abnormality, than flexion or control group.
* Stankovic R, Johnell O: Conservative treatment of Acute Low-Back Pain. A Prospective Randomized Trial: McKenzie Method of Treatment versus patient Education in “Mini Back School”. Spine 15:2, 1990.
The McKenzie method is shown to produce better outcome in 5 of 7 variables compared to a mini back school.
* Stankovic R, Johnell O: Conservative Treatment of Acute Low Back Pain. A 5-Year Follow-up Study of Two Methods of Treatment. Spine 20:4;469-472,1995.
Difference between 2 treatments at 5 years was much less, however McKenzie group had significantly less recurrences of pain and episodes of sick leave.
* Sufka A, Hauger B, Trenary M, Bishop B, Hagen A, Lozon R, Martens B: Centralisation of Low Back Pain and Perceived Functional Outcome. JOSPT 27:205-212, 1998.
Of 36 patients 70% centralised within 14-day test period – centralisation was less amongst those with chronic symptoms and those with more referred pain. Centralisation was associated with significantly more improvement on one of the functional outcome measures used.
Vanharanta H, Videman T, Mooney V: Comparison of McKenzie Exercises, Back Trac and Back School in Lumbar Syndrome; Preliminary Results. Annual Meeting of International Society for the Study of the Lumbar Spine, Dallas, Texas, USA, 1986.
Vanharanta shows the McKenzie method has a greater success in treatment of lumbar pain compared with traction and back school and encourages health professionals to use this line of approach.
* Udermann B, Tillotson J, Donelson R, Mayer J, Graves J. Can an educational booklet change behaviour and pain in chronic low back pain patients? ISSLS, Adelaide, April 2000.
Nine months after reading Treat Your Own Back 81% of 62 recruits with chronic back pain of average 10 years duration were available. About 90% were still using posture and exercise advice from the book, 60% were free of pain, and another 22% had had less pain. Pain severity and number of episodes had significantly improved. Most attributed improvements to what they had learnt in the book.
Underwood MR, Morgan J. The use of a back class teaching extension exercises in the treatment of acute low back pain in primary care. Family Pract 15.1.9-15, 1998.
In an acute group of patients randomised to usual GP care or a back class there were no significant differences in outcome, except one difference at one year, when more of the back class group reported ‘back pain no problem in previous 6 months’.
* Werneke M, Hart DL, Cook D: A descriptive study of the Centralisation Phenomenon. A Prospective Analysis. Spine 24.676-683, 1999.
Of 289 patients with acute neck and back pain 31% centralised during repeated movement testing in the clinic and achieved abolition of symptoms on an average of 4 sessions; 46% showed some centralisation or reduction of symptoms on an average of 8 sessions (partial response); 23% showed no change in symptom site or intensity over an average of 8 sessions. The authors question whether in the partial response group changes were a product of the natural history or exercise programme. Both centralisers and partial responders showed significant improvement in pain intensity and function. Assessment of initial pain location was reliably assessed.
* Williams M M, Hawley J A, McKenzie R A. Van Wijmen P M: A Comparison of the Effects of Two Sitting Postures on Back and Referred Pain. Spine 16:10; 1185-1191, 1991.
Over a 24-48 hour period 2 groups of patients with back and referred pain were encouraged to sit in lordosis or in a kyphotic posture. Lordotic sitting group had back and leg pain significantly reduced and pain centralised compared to kyphotic group.
Williams M, Grant R: Effects of a McKenzie spinal therapy and rehabilitation programme: preliminary findings. The Society for Back Pain Research (UK). Annual Scientific Meeting. (Abstract), 1992.
Significant change in pain, function and psychological status in chronic low back pain patients was found following a 2 week residential programme based on the McKenzie method of treatment.
Williams M M, Grant R N: A comparison of low-back and referred pain responses to end-range lumbar movement and position. Conference Proceedings of the International Society for the Study of the Lumbar Spine, Chicago, USA, May 20-24, 1992.
The importance of monitoring changes in the distal symptoms is highlighted in a prospective trial comparing two forms of repeated end range exercises.
Battie MC, Cherkin DC, Dunn R, Ciol MA, Wheeler KJ: Managing Low Back Pain: Attitudes and Treatment Preferences of Physical Therapists. Physical Therapy 74. 219-226, 1994.
A survey of therapists in USA when presented with hypothetical back pain patients. The McKenzie method was deemed the most useful method of managing patients, and was said to be a very common means of evaluating patients.
Foster NE, Thompson KA, Baxter GD, Allen JM: Management of Nonspecific Low Back Pain by Physiotherapists in Britain and Ireland. A Descriptive Questionnaire of Current Clinical Practice. Spine 24.1332-1342, 1999.
The McKenzie method was said to be the second most common treatment approach used by therapists. The Mait land approach was used by 59%, McKenzie method by 47%,, multiple other approaches were used as well with less frequency – combined approaches were common.
McKenzie R A: Prophylaxis in Recurrent Low Back Pain. NZMedJ no 627, 89:22-23, 1979.
Frequent restoration of the lumbar lordosis and avoidance of flexion were seen as critical factors in prophylactic education for prevention of recurrent LBP. McKenzie reports on 318 patients – onset, aggravating and relieving factors, deformity, and the success of treatment in reducing further attacks as reported by the patients.
Rath W W, Rath J N D, Duffy C G: A comparison of Pain Location and Duration with Treatment Outcome and frequency. Presented at first international McKenzie Conference, Newport Beach, CA, July 1989.
Rath’s retrospective study shows that 87% of lumbar and cervical pain patients had good outcome using the McKenzie method of treatment.
Rath W, Rath JD: Outcome assessment in clinical practice. McKenzie Institute (USA) Journal 4:3;9-16, 1996.
This retrospective study shows how neurological signs, chronicity of the problem, no centralisation, mechanically inconclusive findings on assessment, and positive behavioural signs tend to be associated with a less good outcome. This survey also reports on number of visits related to QTF categories, and the results of a telephone follow-up of patients at least a year after discharge asking about recurrences and ability to self-treat.
Laslett M, Michaelsen DJ, Williams MM: A survey of patients suffering mechanical low back pain syndrome OR sciatica treated with the “McKenzie method”. NZ J Physiotherapy 24-32, August 1991.
A retrospective postal survey of patients’ opinions about the success of treatment in dealing with their present pain, and enabling them to deal with recurrences showed high levels of satisfaction. Derangements 1 & 3 required fewer treatment sessions than Derangements 4,5,6.
Donahue MS, Riddle DL, Sullivan MS: Intertester Reliability of a Modified Version of McKenzie’ Lateral Shift Assessments Obtained on Patients with Low Back Pain. Physical Therapy 76:7;706-726, 1996.
Determination of a lateral shift by observation was found to be very unreliable. Determination of positive side-gliding test, based on alteration of patient’s pain, was found to be of high reliability.
* Donelson R, Aprill C, Medcalf R, Grant W, A prospective study of centralisation of lumbar and referred pain. A predictor of symptomatic discs and anular competence. Spine, 22, 10, 1115-1122, 1997
A confirmation that the McKenzie assesssment is a reliable process to differentiate discogenic from non-discogenic pain and is superior to MRI scanning in distinguishing painful from non-painful discs.
Fiebert I, Keller CD: Are “passive” Extension Exercises Really Passive? JOSPT 19:2;111-115, 1994.
During EIL there is more EMG activity in the Erector Spinae muscles than during standing, EIS, or prone lying.
Fritz JM, Delitto A, Vignovic M, Busse RG. Interrater reliability of judgements of the centralisation phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil 81,57-61, 2000.
40 students and 40 physical therapists reviewed a composite videotape made during assessment of back pain patients and had to make judgements on changes in pain status with movement testing. Intertester reliability was excellent, kappa = 0.79.
Karas R, McIntosh G, Hall H, Wilson L, Meles T: The Relationship Between Nonorganic Signs and Centraliazation of Symptoms in the Prediction of Return to Work for Patients with Low Back pain. Physical Therapy 77:4;354-360, 1997.
Inability to centralize indicated a decreased probability of returning to work, regardless of the Waddell score. A high Waddell score predicted a poor chance of returning to work regardless of the patients’ ability to centralize symptoms. Waddell scores appear to be a better predictor of poor outcomes.
* Kilby J, Stigant M, Roberts A: The Reliability of Back Pain Assessment by Physiotherapists, Using a ‘McKenzie Algorithm’. Physiotherapy 76:9;579-583, September 1990.
Kilby presents a McKenzie algorithm which was found to be intertester reliable, except with regard to identifying the presence of a lateral shift or a kyphotic lumbar spine.
Laslett M, Williams M, The reliability of selected pain provocation tests for sacroiliac joint pathology, Spine, 19, 11, 1243-1249, 1994
Five of the seven tests were shown to be reliable, and may be used to detect a sacroiliac cause of low back pain. They were the distraction (or gapping) test, compression test, posterior shear (or thigh thrust) test, left and right pelvic torsion (or Gaenslen’s) test.
McKenzie R A: Manual Correction of Sciatic Scoliosis. NZMedJ no 484, 76:194-199, 1972.
McKenzie outlines the treatment procedure for manual correction of sciatic scoliosis.
Mulvein K, Jull G: Kinematic analysis of the lumbar lateral flexion and lumbar lateral shift movement techniques. J Manual Manip Ther 3:3;104-109,1995.
Lateral shift technique (side gliding in standing) is found to produce movement with greater specificity to lower lumbar levels compared to lateral flexion. Above L4 either test movements can be used to examine movement abnormalities.
Razmjou H, Kramer JF, Yamada R: Intertester reliability of the McKenzie evaluation in assessing patients with mechanical low-back pain. JOSPT 30,368-389, 2000.
Two physical therapists, one assessor, one observer, both experienced in McKenzie assessed 45 subjects and were analysed on agreements using Kappa statistics. Agreement on syndromes was good (93%), derangement sub-syndrome classification was excellent (97%), presence of lateral shift was moderate (78%), relevance of lateral shift and lateral component was very good/excellent (98%), deformity in sagital plane was excellent (100%).
Riddle D L, Rothstein JM: Intertester Reliability of McKenzie’s classification of the type of the syndrome types present in patients with low back pain. Spine 18:10;1333-1344, 1993.
Riddle found that intertester reliability using his version of the McKenzie system is poor when determining the diagnosis of a patient with low back pain.
Riddle DL: Classification and Low Back Pain: A review of the literature and Critical Analysis of Selected Syndromes. Physical Therapy 78:7;708-737, 1998.
Critical analysis of various classification systems used for LBP, including McKenzie’s. Highlights strengths and weaknesses of them according to an established set of criteria for appraising classification systems.
Roach KE, Brown M, Dumigan KM, Kusek CL, Walas M: Test-retest reliability of a low back pain questionnaire. Physical Therapy 74:5,S56, 1994.
Patient reports concerning leg pain were generally more reliable than back pain. Reports of back and leg pain, with one exception, had good reliability as examined using the Kappa coefficient.
Sallade J: Variation on Robin McKenzie’s technique for correction of lateral shift. J Orth Sports Phys Ther 8:8;417-420,1987.
Author presents his own version of correcting the lateral shift with patient hanging by arms from overhead bar.
Spratt K F, Lehmann T R, Weinstein J N, Sayre H A: A New Approach to the Low-Back Physical Examination. Behavioural Assessment of Mechanical Signs. Spine 15:2, 1990.
The presence of various behavioural responses to pain during physical examination may help to determine outcome of treatment, endorse physical signs and confirm diagnosis. Used repeated movements for some tests. Intertester agreement for patient reported pain status was nearly perfect.
Stankovic R, Johnell O, Maly P, Willner S: Use of lumbar extension, slump test, physical and neurological examination in the evaluation of patients with suspected herniated nucleus pulposus. A prospective clinical study. Manual Therapy 4:25-32, 1999.
105 patients were diagnosed by CT and/or MRI as having disc hernia (N=52), bulging discs (41), or without positive findings (12). A range of clinical and physical examination findings was generally unable to distinguish between these diagnoses. The only 3 variables that were of diagnostic value were ROM on flexion, side bending, and pain distribution on EIS. Neurological tests, EIL (not reported if single or repeated), and SLR were amongst the numerous variables that failed to be associated with any particular diagnosis.
Tenhula JA, Rose SJ, DelittoA: Association Between Direction of lateral Shift, Movement Tests, and Side of symptoms in Patients with low Back Pain Syndrome. Physical Therapy 70:480-486, 1990.
There was no significant relationship between the side of symptoms and the direction of the shift. Contralateral side bending was significantly more likely to provoke symptoms than ipsilateral.
Weitz EM: The Lateral Bending Sign. Spine 6:388-397, 1981.
Study using dynamic lateral bending radiographs to localise disc lesions associated with a shift or reduced lateral bending.
Williams M M, McKenzie R A, Reed R, Laslett M: Responsiveness to Change of Three Disability Assessment Instruments for Back Pain Research. Presented at International Society for the Study of the Lumbar Spine Meeting, Heidelberg, May 12-16, 1991.
Williams concludes that with chronic back pain patients the Dallas pain questionnaire is most sensitive to small changes compared with the Rolland and Oswestry questionnaires.
Williams M M, Wright D G R, Mugglestone A A, Lynch G B, Spekreijse S A: Psychological distress in chronically disabled workers attending a McKenzie spinal therapy and rehabilitation programme. The New Zealand Pain Society. Annual Scientific Meeting. Conference proceedings (Abstract), 1993.
The Distress and Risk Assessment Method (DRAM) appears to have predictive value for treatment outcome in a chronically disabled low back pain population.
Adams MA, Hutton WC. Prolapsed intervertebral disc. A hyperflexion injury. Spine 10. 184-191, 1982.
Cadaveric experiment simulating hyperflexion led to disc failure by posterior prolapse in 26 out of 61 motion segments tested.
Adams MA, Hutton WC. The effect of fatigue on the lumbar intervertebral disc. JBJS 65B. 199-203, 1983.
Cadaveric experiment simulating a vigorous day’s activity in flexion led to fatigue failure of annulus, with distortion of the lamellae and fissures in 23 out of 41 motion segments tested.
Adams MA, Hutton WC. Gradual disc prolapse. Spine 10.524-531, 1985.
Cadaveric experiment loading motion segments in compression and bending caused 6 out of 52 to gradual prolapse, starting with distortion of the lamellae and progressing to nuclear herniation. The most common mechanism of failure was end-plate fracture.
Adams MA, Dolan P. Recent advances in lumbar spinal mechanics and their clinical significance. Clin Biomech 10.3-19, 1995.
Comprehensive review of how spinal structures fail (over 200 refs) with emphasis on importance of mechanical loading in back pain. Discs particularly prone to fatigue failure.
Adams MA, May S, Freeman BJC, Morrison HP, Dolan P. Effects of backward bending on lumbar intervertebral discs. Relevance to therapy treatments for low back pain. Spine 25.4.431-437, 2000.
Cadeveric experiment in which the distribution of compressive stresses within ‘degenerated’ discs were measured by dragging a stress transducer through it. Extension caused an average increase in localised stress peaks in the posterior annulus, however in 7/19 discs extension caused a decrease in stress peaks by up to 40%. It was hypothesised that this reduction was due to stress shielding by the neural arch in more degenerated discs.
Beattie PF, Brooks WM, Rothstein JM et al: Effect of Lordosis on the Position of the Nucleus Pulposus in Supine Subjects. A Study Using MRI. Spine 19:18;2096-2102, 1994.
In vivo some anterior displacement of the nucleus pulposus with extension movements was observed. Degenerated discs appear to behave differently from non-degenerated discs.
Boissonnault W, Di Fabio RP. Pain profiles of patients with low back pain referred to physical therapy. JOSPT 24,4,180-191, 1996.
98 patients with chronic back pain surveyed about aggravating and relieving factors etc. Pain was worse in morning and evening, and commonest aggravating factors were sitting, driving, bending, and lifting. Commonest alleviating postures were recumbency, changing positions, and walking. Non-serious night pain was common.
Fennell AJ, Jones AP, Hukins DWL: Migration of the Nucleus Pulposus Within the Intervertebral Disc during Flexion and Extension of the Spine. Spine 21:23;2753-2757, 1996.
In vivo flexion tends to cause posterior displacement of the nucleus pulposus and extension anterior displacement using MRI.
Kuslich, S D, Ulstrom C L, Michael C J: The Tissue Origin of Low Back Pain and Sciatica: A Report of Pain Response to Tissue Stimulation During Operations on the Lumbar Spine Using Local Anasthesia. Orthop Clinics of North America 22:2;181-187, 1991.
When mechanically stimulated during an operation the outer annulus, posterior longitudinal ligament, vertebral end plate, anterior dura and previously traumatised nerve roots, were all pain sensitive.
Magnusson M, Aleksiev AR, Spratt KF, Lakes RS, Pope MH: Hyperextension and spine height changes, Spine, 21, 22, 2670-2675, 1996
Hyperextension was demonstrated to be a beneficial movement to unload the spine after loading, aiding rehydration and concomitant improvement of disc nutrition.
Reddeck T: An evaluation of the McKenzie regimen – validity of the disc model. Proceedings 10th Biennial Conference of Manipulative Physiotherapists Association of Australia. November 26-29, Melbourne, Australia, 1997.
This paper reviews the disc as a source of pain, the role of annular fissuring and displacement as a mechanism of pain production, and the relationship between the degree of disc pathology and the extent of symptoms.
Schnebel BE, Simmons JW, Chowing J, Davidson R: A digitizing technique for the study of movement of intradiscal dye in response to flexion and extension of the lumbar spine. Spine 13:3;309-312.
Nuclear material in normal discs moves anteriorly with extension and posteriorly with flexion, however movements in degenerated discs were less predictable.
Schnebel B E, Watkins R G, Dillin W: The Role of Spinal Flexion and Extension in Changing Nerve Root Compression in Disc Herniations. Spine 14:8;835-837, 1989.
Using cadaver models of herniated discs, Schnebel demonstrated that flexion increases tension and that extension decreases tension on the L5 nerve root.
Shepherd J: In vitro study of segmental motion in the lumbar spine. JBJS 77B: S2,161, 1995.
Intradiscal material generally moved anteriorly on extension and posteriorly in flexion, but amount varied amongst the specimens.
Vanharanta H, Ohnmeiss D, Rashbaum R et al: Effect of Repeated Trunk Extension and Flexion Movements as seen by CT/Discography. Orthopaedic Transactions 12:3;650-651, 1988.
No change observed in position of nucleus pulposus after flexion or extension.
DiMaggio A, Mooney V: The McKenzie Program: Exercise effective against back pain. Journ Musculoskel Med 4:12;63-74, 1987.
The authors provide a review of the McKenzie assessment and treatment protocol and its rationale.
Donelson R: The McKenzie approach to Evaluating and Treating low back pain. Orthopaedic Review, Vol XIX, No 8, August 1990.
Donelson presents an overview of the McKenzie approach to low back pain treatment.
Donelson R G, McKenzie R: Mechanical Assessment and Treatment of Spinal pain. In: The Adult Spine: Principles and Practice. Editor-in-Chief J W Frymoyer. New York:Raven Press Ltd 1991. Vol Two, Chapter 76:1627-1639.
A review of the McKenzie assessment and treatment philosophy is provided along with a review of the relevant research pertaining to the method.
Donelson R G: Identifying appropriate exercises for your low back pain patient. Journ Musculoskel Med, pp 14-29, December 1991.
Donelson provides an overview of the McKenzie approach and reports on its success rates.
Grant R N, McKenzie R A: Mechanical Diagnosis and Therapy for the Cervical and Thoracic Spines. In: Clinics in Physical Therapy series: Physical Therapy of the Cervical and Thoracic spine, 2nd ed. Ed Prof Ruth Grant, University of South Australia.
An overview of the McKenzie approach with specific reference to the cervical and thoracic spine.
Holdom A. The use of McKenzie approach to treat back pain. Br J Ther & Rehab. 3.1.7-10, 1996.
Overview of mechanical diagnosis, centralisation, force progressions, and value of approach in offering self-management.
Hyman MH, Jacob G, Lin K, Mooney V. Primary care update: brief summaries for clinic. Mechanical diagnosis and therapy: the McKenzie approach to spinal complaints. Consultant 39.7.2115-6, 1999.
Overview.
McKenzie R A: Treat Your Own Back. Spinal Publications, Lower Hutt, N.Z., 1981.
A basic overview of the self-treatment and management of LBP for lay people.
McKenzie R A: Treat Your Own Neck. Spinal Publications, Lower Hutt, N.Z., 1983.
A basic overview of the self-treatment and management of neck pain for lay people.
McKenzie R A: The Lumbar Spine. Mechanical Diagnosis and Therapy. First Edition, Spinal Publications, Lower Hutt, N.Z., 1981.
A description of the McKenzie philosophy outlining assessment, treatment and prophylaxis for low back pain and leg pain.
McKenzie R A: Mechanical Diagnosis and Therapy for Low Back Pain: Towards a better understanding. In: Clinics in Physical Therapy. Physical Therapy of the Low Back, p157. Ed LT Twomey and JR Taylor. Churchill Livingstone, 1987.
McKenzie challenges the physiotherapy profession to critically look at the history of manipulative therapy, to learn from it, and to adopt a more organised rational approach to mechanical therapy.
McKenzie R A: The Cervical and Thoracic Spine. Mechanical Diagnosis and Therapy. First Edition, Spinal Publications (N.Z.) Ltd, Waikanae, New Zealand, 1990.
A revision and update of the McKenzie method of mechanical diagnosis and therapy with specific reference to the cervical and thoracic spine.
McKenzie R A: Mechanical Diagnosis and Therapy for Low Back Pain: Towards a better Understanding. In: The Lumbar Spine. Eds James Weinstein and Sam Weisel. Philadelphia: W B Saunders Company, 1990, Chapter 16, pp 792-805.
McKenzie reviews his classification system and emphasises the need for self-treatment.
McKenzie R A: A Physical Therapy Perspective on Acute Spinal Disorders. In; Contemporary Conservative Care for Painful Spinal Disorders: Concepts, Diagnosis and Treatment. Ed T G Mayer, V Mooney, R J Gatchel. Malvern, PA: Lea & Febiger, 1991, pp 211-220.
McKenzie compares his system of classification to the Quebec task Force findings.
McKenzie R A: Spinal Assessment and Therapy Based on the Behaviour of Pain and Mechanical Response to Dynamic and Static Loading. In: Proceedings of Advances in Idiopathic Low Back Pain Symposium, Vienna, Austria, Nov 27-28, 1992. Ed Prof DDr E Ernst.
A review of the Quebec Task Force findings and the McKenzie classification system, incorporating an introduction to the use of REPEX to facilitate the treatment process.
McKenzie R A: Mechanical Diagnosis and Therapy for Disorders of the Lower Back. In: Clinics in Physical Therapy. Physical Therapy of the Low back. 2nd ed. Eds L T Twomey and J R Taylor. Churchill Livingstone. 1994
Mooney V. Treating low back pain with exercise: the McKenzie approach. J Musculo Med 12.12.24-6,28,33-36, 1995.
Overview.
Poulter D C, McKenzie R A: The Management of Work Related Back Pain. In: Patient Management. Auckland NZ: Adis International Medical Publishers. (in press).
The authors suggest common causes of LBP in the work-place. They provide a review of tissue healing and suggest that self treatment exercises can be used in the work-place to prevent recurrence.
Stevens B J, McKenzie R A: Mechanical Diagnosis and Self Treatment of the Cervical Spine. Clinics in Physical Therapy, Vol 17: Physical Therapy of the Cervical and Thoracic spine, ed Ruth Grant. Churchill Livingstone Inc, 1988.
A review of the McKenzie mechanical syndromes, patient evaluation, treatment progression, and prophylaxis as it pertains to the cervical spine.
Taylor MD. The McKenzie method: a general practice interpretation. The lumbar spine. Aust Fam Phys 25.2.189-20 1, 1996.
Overview of mechanical diagnosis and therapy in which the author proposes alternative nomenclature for mechanical syndromes – namely incipient trauma (posture), unhealed trauma (derangement), and healed trauma (dysfunction).
Van Wijmen P M: Lumbar Pain Syndromes. In: Grieve GP (ed). Modern Manual Therapy of the Vertebral Column. Churchill Livingstone, New York, 1986. Ch 41:442-462.
A detailed overview of the McKenzie approach to treating low back pain.
Van Wijmen P M: The management of recurrent low back pain. In: Grieve GP (ed). Modern Manual Therapy of the Vertebral Column. Churchill Livingstone, New York 1986. Ch 73:756-776.
Outlines that the self treatment approach should be the key management strategy for low back pain.
Jacob G:The McKenzie Protocol and the Demands of Rehabilitation. California Chiropractic Association Journal 16:10, October 1991.
Jacob likens the McKenzie approach and chiropractic approach and states that movement is the key to pain relief, either using patient generated forces or therapist generate forces when required.
Jacob G: Specific application of movement and positioning technique to the lumbar spine, considering theoretical formulation and therapeutic application. Today’s Chiropractic, Part I, Vol 18, No 6; Part II, Vol 19, No 1, 1989-90.
The rationale for flexion procedures is outlined which has resulted in a failure to adequately explore the relationship of pain behaviour to movement and positions of the lumbar spine.
Jacob G: Spinal therapeutics based on responses to loading. 4th Mckenzie Institute International Conference, Cambridge, 16-17 September, 1995.
Discussion of mechanical and symptomatic responses to different loading strategies.
McKenzie R: A Perspective on Manipulative Therapy. Physiotherapy 75:8, 1989, pp 440-444.
McKenzie presents a review of spinal manipulative therapy and suggests that therapist generated forces should only be indicated when patient generated forces have been exhausted.
Mooney V: Reducing Subacute and Chronic Low back disability. Guest editorial in Orthopaedic Review, Vol XIX, No 8, August 1990.
Mooney concludes that active patient participation, early care and evaluation of function but not pain results in good outcomes when treating low back pain.
Watson G: Neuromusculoskeletal physiotherapy: Encouraging self-management. Physiotherapy 82:6;352-357.
Watson urges that physiotherapists should promote a therapeutic alliance with patients to encourage self-management, an approach that is efficient, increases patient compliance, and helps prevent recurrences.
- Cervical Spine - Systematic Reviews
- Cervical Spine - Trials
- Cervical Spine - Anatomical Physiological Pain Studies
- Cervical Spine - Whiplash
- Cervical Spine - Correspondence
Aker PD, Gross AR, Goldsmith CH, Peloso P. Conservative management of mechanical neck pain: systematic overview and meta-analysis. BMJ 313.1291-1296, 1996.
Review of 24 RCTs: positive treatment effect for manual therapy from pooled results; for passive therapies, drug treatment and education results are contradictory and inadequate to reach conclusions.
Coulter I. Manipulation and mobilization of the cervical spine: the results of a literature survey and consensus panel. J Musculo Pain 4.113-123, 1996.
Review of 14 RCTs: for acute and chronic neck pain manual therapy may have some positive treatment effect, where tested exercises are as effective.
Di Fabio RP. Manipulation of the cervical spine: risks and benefits. Phys Ther 79.50-65, 1999.
Review of 12 RCTs: manual therapy has a positive treatment effect, with no proven difference between mobilisation and manipulation.
Hurwitz EL, Aker PD, Adams AH, Meeker WC, Shekelle PG. Manipulation and mobilisation of the cervical spine. A systematic review of the literature. Spine 21.1746-1760, 1996.
Review of 14 RCTs, plus other studies, favouring short-term treatment effect of manual therapy.
Kjellman GV, Skargren EI, Oberg BE. A critical analysis of RCT on neck pain and treatment efficacy. A review of the literature. Scand J Rehab Med 31.139-152, 1999.
Review of 27 RCTs: positive outcomes and good quality studies supporting ‘active’ physiotherapy, manipulation, electromagnetic therapy.
* Abdulwahab SS, Sabbahi M. Neck retractions, cervical root decompression, and radicular pain. JOSPT 30.1.4-12, 2000.
In a group of patients with neck and radicular pain a posture of sustained flexion caused a significant increase in peripheral pain and root compression as measured by H reflex amplitude. Repeated retractions caused a significant decrease in peripheral pain and decrease of nerve root compression.
Donelson R, Grant W, Kamps C, Richman P. Cervical and referred pain response to repeated end-range testing: a prospective, randomised trial. Nth Am Spine Soc. New York, 1997.
In patients with neck and referred symptoms 45% had pain reduced or centralised with sagital plane movements. Of this group 67% had a preference for extension and retraction and 33% had a preference for flexion and protrusion. In the remaining patients 14% showed a preference for extension, but not retraction, and 12% were worse with flexion, but not better with extension.
Hanten WP, Barrett M, Gillespie-Plesko M, Jump KA, Olson SL. Effects of active head retraction with retraction/extension and occipital release on the pressure pain threshold of cervical and scapular trigger points. Physio Theory & Pract 13.285-291, 1997.
One session of either intervention caused no significant changes in trigger point sensitivity.
See also: Werneke et al 1999. In ‘Trials’ lumbar spine.
Cloward RB: Cervical discography. A contribution to the aetiology and mechanism of neck, shoulder and arm pain. Ann of Surg 150:1052-1064,1959.
At surgery stimulation of cervical discs produced intra-scapular pain, with stimulation mid-line producing central pain and off-centre producing lateral pain.
Donelson R: Cervical protrusion and retraction. McKenzie Institute (UK) Newsletter 3:2;20-21,1994.
A radiographic and range of movement study of the effects of protrusion/retraction, and an analysis of symptom response to sagital end-range test movements. Of the 45% who experienced improvement “directional preference” was for extension in 67%, and for flexion in 33%.
Harms-Ringdahl K. On assessment of shoulder exercise and load elicited pain in the cervical spine. Scand J Rehab Med S14.1-40, 1986.
Various motor and sustained loading tests carried out on asymptomatic volunteers. When sustaining extreme flexion pain was produced after 2-15 minutes and stopped test within hour, when the pain abated. Pain was mostly neck and shoulders.
Mercer SR, Bogduk N: The Ligaments and Annulus of Human adult Cervical Intervertebral Discs. Spine 24: 7, 619-628, 1999
The three-dimensional architecture of the cervical annulus fibrosis is more like a crescentic anterior interosseous ligament than a ring of fibres surrounding the nucleus pulposus.
Mercer SR, Jull GA: Morphology of the cervical intervertebral disc: implications for McKenzie’s model of the disc derangement syndrome. Manual Therapy 1:2;76-81, 1996.
As the morphology and degenerative process of the cervical spine is different from the lumbar spine the authors conclude that the model does not conform to known anatomy. (see also discussion McKenzie Institute (UK) Newsletter 5:1;10-14,1996)
Ordway NR, Seymour RJ, Donelson RG, Hojnowski LS, Edwards WT: Cervical Flexion, Extension, Protrusion, and Retraction. A Radiographic Segmental analysis. Spine 24:240-247, 1999.
Study into the paradoxical movement pattern of the cervical spine – retraction produces lower C extension and upper C flexion, protrusion produces lower C flexion and upper C extension. Full range extension is produced in lower C by extension, but in O-C2 by protrusion; full range flexion is produced in lower C by flexion, but in O-C2 by retraction.
Pearson ND, Walmsley RP: Trial into the effects of repeated retractions in normal subjects. Spine 20:11;1245-1251,1995.
Retraction range did not increase on repetition, and range was greater in the younger population.
Schellhas KP, Smith MD, Gundry CR, Pollei SR: Cervical discogenic pain. Prospective correlation of MRI and discography in asymptomatic subjects and pain sufferers. Spine 21:3;300-312,1996.
Most cervical discs are morphologically abnormal, with outer annular tears found in both volunteers an d patients. Gives areas of referral for discogenic pain.
Barnsley L, Lord S, Bogduk N: Clinical review: Whiplash injury. Pain 58;283-307, 1994.
Thorough review of epidemiology, pathology, symptoms and litigation issue. Studies show that about a quarter will continue to have persistent pain.
Borchgrevink GE, Kaasa A, McDonagh D et al: Acute treatment of whiplash neck sprain injuries. A randomised trial of treatment during the first 14 days after a car accident. Spine 23:25-31, 1998.
Continuing to engage in normal activities led to fewer symptoms than did sick leave and use of a collar.
Freeman MD, Croft AC, Rossignol AM; “Whiplash associated disorders: redefining whiplash and its management” by the QTF. A critical evaluation. Spine 23:1043-1049,1998.
Critical appraisal of Spitzer (1995) showing that their conclusions about the self-limiting/ favourable prognosis is not born out by the literature. In fact about 33% of whiplash patients have persistent pain several years later.
McKinney L A: Early mobilisation and outcome in acute sprains of the neck. Brit Med J 299:1006, 1989.
A single advice session produced fewer patients with persistent symptoms at 2 years than a course of manipulative physiotherapy. Prolonged collar-wearing is associated with persistence of symptoms.
McKinney L A, Dornan J O, Ryan M: The Role of Physiotheraphy in the management of acute neck sprains following road-traffic accidents. Archives of Emergency Medicine 6:27-33, 1989
Outpatient treatment and advice to mobilise earlier were both more effective than analgesics and a collar in treating acute neck sprains.
Mealy K, Brennan H, Fenelon GCC: Early mobilisation of acute whiplash injuries. BMJ 292: 656-657, March 1986.
Early active mobilisation and exercises produced significantly less pain and improved movement compared to rest and use of a collar.
Spitzer WO, Skovron ML, Salmi LR et al: Scientific Monograph of the Quebec task Force on Whiplash-Associated Disorders: Redefining Whiplash and its Management. Spine 20;1S-73S,1995.
An extensive review of the problem condoning an active, exercise, early return to normal function approach; stressing the self-limiting, favourable prognosis of the condition.
Cherkin study (1998). NEJM 340.5.388-391, 1999.
Delitto A, Cibulka M T, Erhard R E, Bowling R W, Tenhula J A: Author response. Physical Therapy 73:4;226, 1993.
The authors claim that they are testing the effect of treatment to a diagnostic classification, not the McKenzie method.
Donelson R, McKenzie R: Letter to the Editor, Spine 17:10;1267, 1992.
In reference to the study by Elnaggar I M, et al: Effects of Spinal Flexion and Extension Exercises on Low-Back Pain and Spinal Mobility in Chronic Mechanical Low-Back Pain patients. Spine 16:8;967-972, 1991.
The authors explain that extension exercises have been used, not the McKenzie approach in comparison with spinal flexion exercises.
Fernando CK. Donelson R. Spine 16.1008-1009, 1991.
2 letters concerning Stankovic trial (Spine 15:120-123, 1990).
Long A. More on centralisation. JOSPT.29.8.489-490, 1999.
Silva GJ. Riddle DL & Rothstein JM. Donelson R. Spine 19:12;1413-1415, 1994.
Correspondence concerning Riddle & Rothstein paper (Spine 18:1333-1344, 1993).
Williams M M, McKenzie R A, Farrell J P: Commentaries. Physical Therapy 73:4;223, 1993.
McKenzie and Williams point out some inconsistencies and inadequacies with Delitta’s study, but commend the authors on the study and agree that further research needs to be done.
Dersom manglende litteratur under de ulike kategoriene, vennligst ta kontakt på pm så skal jeg ta det med i den oversikten.
Konklusjon
McKenzie-metoden eller Mekanisk Diagnostikk og Terapi (MDT) er en internasjonal annerkjent metode for diagnostikk og behandling rettet mot ryggrad og ekstremitetssmerter. MDT brukes i dag av flere profesjoner, som enten brukes metoden i sin helhet (MDT-praktikere) eller elementer av den (manuelterapeuter og spesialister i ortopedisk fysioterapi). Hjertebarnet til McKenzie ligger i mobiliseringsøvelser og filosofien bak MDT ligger i «aktiv pasientinvolvering og skolering». Den fullstendige McKenzie-metoden består av tre ledd, som omfatter i) Undersøkelse, ii) Behandling og iii) Forebygging.
McKenzie-metoden er ikke effektiv for alle pasienter, dvs at ikke alle vil oppleve bedring av symptombildet. Dette i og for seg er et viktig funn å ta i betraktning for å adressere hvilke pasienter vil ha nyte av MDT og hvilke som har behov for annen tilnærming.
Robin McKenzie regnes som en av de som har hatt mye inflyttelse og fått mye oppmerksomhet innenfor fysioterapi. Hans tilnærming er klassifisert som mer mekaniskrettet ift undersøkelse, interpretering eller behandling. Andre personligheter med lignende innflyttelse innenfor fysioterapi er James Cyriax, Florence Kendall, Geoffrey Maitland, Stanley Paris, Shirly Sahrmann og Brian Mulligan.
Referanser
Brennan, G. P., Fritz, J. M., Hunter, S. J., Thackeray, A., Delitto, A., & Erhard, R. E. (2006). Identifying Subgroups of Patients With Acute/Subacute “Nonspecific” Low Back Pain (Results of a Randomized Clinical Trial). Spine, 31(6), 623–631. https://doi.org/10.1097/01.brs.0000202807.72292.a8
Clare, H. A., Adams, R., & Maher, C. G. (2005). Reliability of McKenzie classification of patients with cervical or lumbar pain. Journal of Manipulative and Physiological Therapeutics, 28(2), 122–127. https://doi.org/10.1016/j.jmpt.2005.01.003
Donelson, R., Silva, G., & Murphy, K. (1990). Centralization phenomenon. Its usefulness in evaluating and treating referred pain. Spine. https://doi.org/10.1097/00007632-199003000-00010
Garcia, A. N., Gondo, F. L., Costa, R. A., Cyrillo, F. N., Silva, T. M., Costa, L. C., & Costa, L. O. (2011). Effectiveness of the back school and mckenzie techniques in patients with chronic non-specific low back pain: a protocol of a randomised controlled trial. BMC Musculoskeletal Disorders, 12(1), 179. https://doi.org/10.1186/1471-2474-12-179
Hefford, C. (2008). McKenzie classification of mechanical spinal pain: Profile of syndromes and directions of preference. Manual Therapy, 13(1), 75–81. https://doi.org/10.1016/j.math.2006.08.005
Machado, L. A. C., de Souza, M. V. S., Ferreira, P. H., & Ferreira, M. L. (2006). The McKenzie method for low back pain: a systematic review of the literature with a meta-analysis approach. Spine, 31(9), E254–E262. https://doi.org/10.1097/01.brs.0000214884.18502.93
Machado, L. A. C., Maher, C. G., Herbert, R. D., Clare, H., & McAuley, J. H. (2010). The effectiveness of the McKenzie method in addition to first-line care for acute low back pain: a randomized controlled trial. BMC Medicine, 8, 10. https://doi.org/10.1186/1741-7015-8-10
May, S. (2006). Classification by McKenzie Mechanical Syndromes: A survey of McKenzie-Trained faculty. Journal of Manipulative and Physiological Therapeutics, 29(8), 637–642. https://doi.org/10.1016/j.jmpt.2006.08.003
May, S., & Donelson, R. (2008). Evidence-informed management of chronic low back pain with the McKenzie method. Spine Journal. https://doi.org/10.1016/j.spinee.2007.10.017
May, S., & Ross, J. (2009). The McKenzie Classification System in the Extremities: A Reliability Study Using Mckenzie Assessment Forms and Experienced Clinicians. Journal of Manipulative and Physiological Therapeutics, 32(7), 556–563. https://doi.org/10.1016/j.jmpt.2009.08.007
McKenzie, R., & May, S. (2003). The lumbar spine: mechanical diagnosis and therapy. Spinal publications Ltd.
Shearer, H. M. (2007). Rehabilitation of the Spine – A Practitioner’s Manual, 2nd Ed. The Journal of the Canadian Chiropractic Association, 51(1), 62. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1924653/